If you are planning spine surgery or recently underwent one, you may be wondering: How long does it take to recover from a Laminectomy? This is one of the most important questions patients ask because recovery directly affects mobility, work, and overall quality of life. While this procedure is highly effective in relieving nerve pressure and improving symptoms, the healing process takes time and varies from person to person.
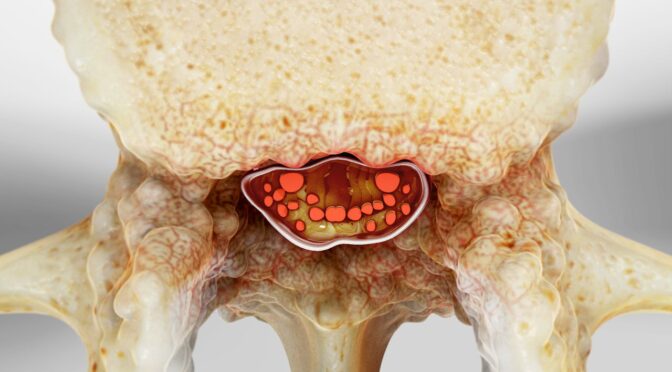
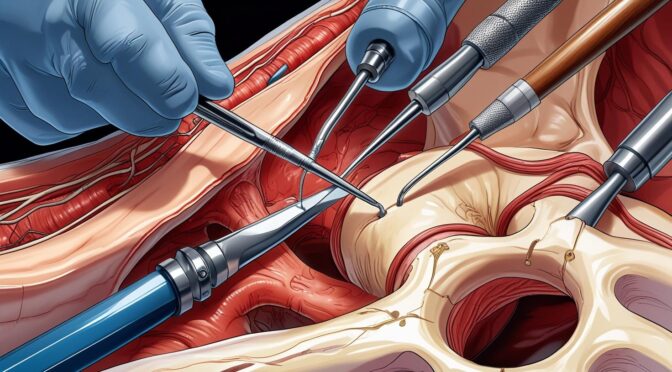
This surgical procedure is performed to relieve pressure on spinal nerves caused by conditions such as spinal stenosis, herniated discs, or bone overgrowth. By removing part of the vertebra, surgeons create more space in the spinal canal, allowing compressed nerves to function normally again. Although the surgery can significantly reduce pain, numbness, and weakness, recovery involves multiple phases that require patience and proper care.
Many patients expect immediate relief, but nerve healing is gradual. Some symptoms improve quickly, while others take weeks or months to fully resolve. Recovery also depends on factors such as age, overall health, physical condition, and whether additional spinal procedures were performed.
In this comprehensive guide, you will learn the complete recovery timeline, what happens during each healing phase, factors that influence recovery speed, and what you can do to accelerate healing safely. Understanding the process helps you set realistic expectations and achieve the best possible outcome.
What Is a Laminectomy and How Does It Affect Recovery?
A Laminectomy is a spinal decompression procedure that removes part or all of the lamina, which is the bony structure covering the back of the spinal canal. This creates more space for the spinal cord and nerves, relieving compression that causes pain, numbness, and weakness. The surgery is commonly performed in the lower back (lumbar spine) but can also be done in the neck or mid-back depending on the location of nerve compression.
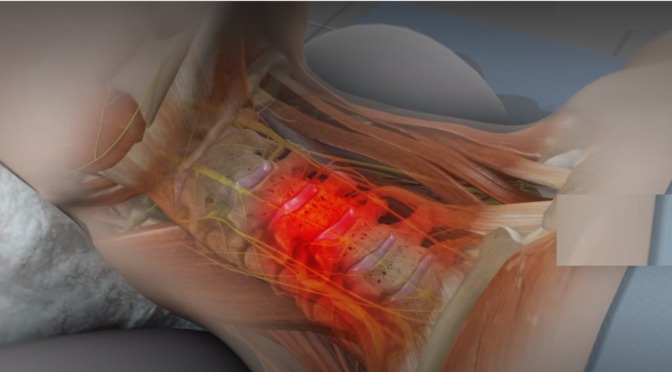
This procedure directly addresses the structural cause of nerve compression rather than just managing symptoms. When nerves are compressed for extended periods, they become inflamed and dysfunctional. Removing the compressive structure allows nerves to recover, but the healing process continues long after the surgery is completed. The body must repair tissues, reduce inflammation, and restore normal nerve function, which explains why recovery takes time.
Recovery also involves healing of muscles, ligaments, and soft tissues that were moved or affected during surgery. Even though modern surgical techniques minimize tissue damage, the body still requires several weeks to repair surgical areas. During this period, patients may experience soreness, stiffness, and fatigue as part of the natural healing process.
According to the Cleveland Clinic, decompression surgery like this procedure significantly improves mobility and reduces nerve-related pain in most patients. However, the timeline varies depending on the severity of nerve compression and the patient’s overall health.
The recovery process can be divided into multiple phases, each with specific healing milestones. Understanding these phases helps patients remain patient and committed to rehabilitation, which is essential for long-term success.
Laminectomy Recovery Timeline: What Happens at Each Stage
Recovery occurs in stages, and each stage represents different healing processes within the body. While some improvements occur quickly, full recovery requires gradual nerve healing and tissue repair.
Immediate Recovery: First 24 to 72 Hours
This is the acute healing phase when the body begins repairing surgical tissues. Patients are closely monitored for complications, and pain management is a priority during this period. Most patients are encouraged to stand and walk within the first day after surgery to promote circulation and prevent complications such as blood clots.
During this phase, patients may experience soreness, stiffness, and fatigue. These symptoms are normal and gradually improve as inflammation decreases. Walking short distances helps improve blood flow, which accelerates healing and reduces stiffness.
Early Recovery Phase: First 2 to 6 Weeks
During this phase, surgical wounds heal, and inflammation continues to decrease. Patients generally experience gradual improvements in pain relief and mobility over time.
Nerve symptoms such as tingling or numbness may improve slowly because nerves heal at a slower rate than other tissues.
Patients are encouraged to increase activity gradually while avoiding heavy lifting or twisting movements. Walking is one of the most effective ways to improve recovery because it strengthens muscles and promotes circulation without placing excessive strain on the spine.
Intermediate Recovery Phase: 6 Weeks to 3 Months
By this stage, most patients experience significant improvement in symptoms and function. Muscles become stronger, and mobility improves considerably. Physical therapy often begins during this period to restore flexibility and strengthen spinal support muscles.
Nerve healing continues during this phase. Some patients notice complete symptom relief, while others experience gradual improvement over several months. The recovery speed depends on how long the nerve was compressed before surgery.
Long-Term Recovery Phase: 3 Months to 1 Year
Full recovery may take several months to a year, especially if nerve compression was severe. During this phase, nerves continue to regenerate and regain normal function. Most patients return to normal activities and experience improved quality of life.
This phase focuses on strengthening the spine and preventing future problems. Maintaining proper posture, staying active, and following medical advice ensures long-term success.
Factors That Affect Laminectomy Recovery Time
Several factors influence how quickly patients recover from spinal surgery. Understanding these factors helps patients set realistic expectations and take steps to improve healing outcomes.
Age and Overall Health
Younger patients generally recover faster because their bodies heal more efficiently. Older patients may take longer due to reduced tissue regeneration and pre-existing health conditions. Chronic illnesses such as diabetes can slow healing by affecting circulation and tissue repair.
Good cardiovascular health improves oxygen delivery to healing tissues, which accelerates recovery. Patients who maintain a healthy lifestyle typically experience smoother and faster healing compared to those with poor health habits.
Severity and Duration of Nerve Compression
The length of time nerves was compressed before surgery significantly affects recovery speed. Nerves that were compressed for shorter periods typically recover faster. Long-term compression may cause nerve damage that takes longer to heal.
In some cases, nerve function continues to improve for months after surgery. This gradual improvement reflects the slow regeneration process of nerve tissue.
Physical Condition and Muscle Strength
Patients with strong muscles and good physical conditioning often recover faster. Strong muscles support the spine and reduce strain during recovery. Weak muscles may require longer rehabilitation to restore stability and function.
Physical therapy helps rebuild strength and improve mobility, which accelerates recovery and prevents complications.
How to Speed Up Laminectomy Recovery Safely
Proper care and rehabilitation play a critical role in recovery speed and long-term success. Following medical recommendations helps prevent complications and improves healing outcomes.
Essential Recovery Strategies
Patients can improve healing and reduce recovery time by following these recommendations:
- Follow all post-surgical instructions carefully
- Attend physical therapy sessions consistently
- Avoid lifting heavy objects during early recovery
- Maintain proper posture while sitting and standing
- Stay physically active with gentle exercises like walking
These actions promote circulation, strengthen muscles, and prevent stiffness, all of which support faster recovery.
Lifestyle Habits That Improve Healing
Certain lifestyle choices significantly influence recovery outcomes:
- Eating a balanced diet rich in nutrients
- Staying hydrated
- Getting adequate rest
- Avoiding smoking
Smoking slows healing by reducing blood flow to tissues. Proper nutrition provides essential nutrients required for tissue repair.
When Can You Return to Normal Activities After a Laminectomy?
Returning to normal activities depends on the healing stage, physical condition, and type of activity. Each activity places different levels of stress on the spine, which influences when it can be safely resumed.
Most patients can begin light activities such as walking within a few days after surgery. Walking helps strengthen muscles, enhances circulation, and reduces stiffness. Gradual activity progression helps rebuild strength without causing strain.
Patients with desk jobs typically return to work within four to six weeks. These jobs place minimal physical stress on the spine, allowing earlier return compared to physically demanding jobs. Patients with physically demanding occupations may require several months before safely returning to work.
Exercise and recreational activities should resume gradually under medical supervision. High-impact activities such as running or heavy lifting require complete healing and strong spinal support muscles. Returning too early increases the risk of complications or reinjury.
Listening to your body and following medical advice ensures safe recovery. Gradual progression prevents strain and supports long-term success.
Signs of Healthy Healing and Warning Signs After a Laminectomy
Understanding normal healing signs helps patients track progress and identify potential complications early.
Signs of Normal Healing
These signs indicate healthy recovery progress:
- Gradual reduction in pain
- Improved mobility
- Increased strength
- Reduced nerve symptoms
These improvements reflect tissue healing and nerve recovery.
Warning Signs That Require Medical Attention
Contact your doctor immediately if you experience:
- Severe or worsening pain
- Fever or signs of infection
- Persistent weakness
- Loss of bladder or bowel control
Early medical intervention prevents serious complications.
Long-Term Outlook After a Laminectomy
Most patients experience significant improvement in symptoms and quality of life after recovery. The procedure effectively relieves nerve compression, allowing patients to regain mobility and function. Long-term success depends on maintaining spinal health through exercise, posture, and healthy lifestyle habits.
Physical therapy strengthens muscles and improves spinal stability, reducing the risk of future problems. Maintaining a healthy weight also reduces stress on the spine and prevents degeneration.
Many patients return to normal activities and enjoy improved mobility and reduced pain. Following medical recommendations ensures lasting benefits and prevents complications.
Conclusion
Recovering from a Laminectomy is a gradual process that involves multiple healing phases, from immediate tissue repair to long-term nerve recovery. While many patients experience symptom relief within weeks, full recovery may take several months depending on individual factors. Following medical advice, staying active, and maintaining a healthy lifestyle significantly improve healing outcomes.
Early rehabilitation and proper care help restore mobility, reduce pain, and improve quality of life. Understanding the recovery timeline helps patients stay informed and confident throughout the healing process. Book your spine consultation today to ensure proper recovery and regain your active, pain-free life.