Have you ever experienced a nagging back pain that seems to worsen when you walk, only to feel relief when you sit down or lean forward on a shopping cart? You’re not alone. This seemingly simple pattern of discomfort could be your body’s way of signalling a condition called spinal stenosis, affecting millions of people worldwide.
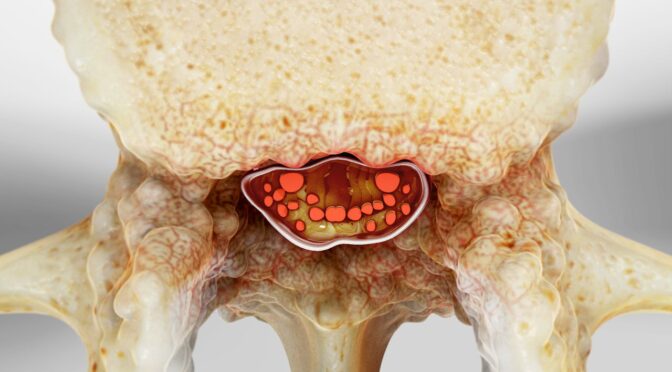
Spinal stenosis is a condition in which the spinal spaces narrow, leading to compression of the nerves within the spine. While this condition often develops gradually over time, recognizing its early warning signs can make a significant difference in your quality of life and treatment outcomes.
Imagine Sarah, a 58-year-old teacher who noticed she could no longer walk the length of the school hallway without stopping to rest. What she initially attributed to aging turned out to be lumbar spinal stenosis. Her story mirrors that of countless individuals who dismiss early symptoms, only to find themselves facing more complex challenges later.
In this comprehensive guide, we’ll explore the critical early warning signs that shouldn’t be ignored, dive deep into the various treatment options available, and provide you with the knowledge needed to take proactive steps toward better spinal health. Whether you’re experiencing symptoms yourself or caring for someone who is, understanding spinal stenosis empowers you to make informed decisions about your healthcare journey.
Understanding Spinal Stenosis: The Foundation of Knowledge
Spinal stenosis represents a narrowing of the spinal canal, the protective tunnel that houses your spinal cord and nerve roots. This narrowing can occur at any level of the spine, but most commonly affects the lumbar (lower back) and cervical (neck) regions.
Types of Spinal Stenosis
The condition manifests in two primary forms, each presenting unique challenges and symptoms:
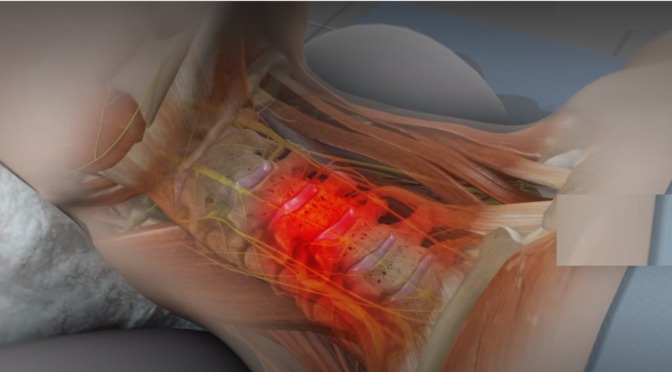
Lumbar spinal stenosis occurs in the lower back and is the type seen most often. Patients typically experience leg pain, weakness, and cramping that worsens with walking or standing upright. The pain often improves when sitting or leaning forward, a phenomenon known as the “shopping cart sign.”
Cervical spinal stenosis occurs in the neck region and can be more serious due to potential spinal cord compression. Symptoms may include neck pain, arm weakness, and in severe cases, problems with balance and coordination.
Primary Causes and Risk Factors
Degenerative, age-related changes constitute the most frequent cause of spinal stenosis. As we age, the ligaments in our spine can thicken, bone spurs may develop, and the discs between vertebrae can bulge or herniate. These changes gradually reduce the space available for nerves.
Other contributing factors include:
- Arthritis: Both osteoarthritis and rheumatoid arthritis can cause inflammation and bone changes
- Congenital conditions: Some individuals are born with naturally narrow spinal canals
- Previous injuries: Trauma from accidents or sports injuries can accelerate degenerative changes
- Tumors: Though rare, growths can compress spinal structures
Recognizing Early Warning Signs: Your Body’s Alert System
Early detection of spinal stenosis symptoms can significantly impact treatment success and prevent progression. Many patients initially dismiss these signs as normal aging, but recognizing patterns can lead to timely intervention.
Lumbar Spinal Stenosis Symptoms
The hallmark symptom of lumbar spinal stenosis is neurogenic claudication – leg pain that develops with walking or standing and improves with sitting or bending forward. This pain pattern distinguishes it from vascular claudication caused by poor circulation.
Key warning signs include:
- Leg cramping or pain that worsens with walking downhill but improves walking uphill
- Sensory changes, including numbness or paraesthesia, in the legs, feet, or buttocks.
- Weakness in the legs that may cause stumbling or difficulty climbing stairs
- Back pain that may be constant or intermittent
- Relief when leaning forward on a shopping cart, walker, or bicycle handlebars
Cervical Spinal Stenosis Symptoms
Cervical spinal stenosis can present more varied and potentially serious symptoms due to the proximity to the spinal cord and brain stem.
Critical warning signs include:
- Neck pain and stiffness that may radiate into the shoulders
- Arm weakness or numbness that can affect fine motor skills
- Hand clumsiness making it difficult to button clothes or write
- Balance problems or unsteady walking
- In serious cases, problems with bowel or bladder control can occur and need urgent medical care.
When to Seek Medical Attention
While mild symptoms may develop gradually, certain red flags warrant immediate medical evaluation. These include sudden onset of severe symptoms, loss of bowel or bladder control, significant weakness in arms or legs, or severe balance problems.
Comprehensive Diagnosis and Assessment Methods
Accurate diagnosis of spinal stenosis requires a thorough evaluation combining clinical assessment with advanced imaging techniques. Healthcare providers use a systematic approach to confirm the diagnosis and determine the extent of nerve compression.
Clinical Evaluation Process
The first step in finding the cause is talking about your health history and having a physical check-up. Your healthcare provider will assess your symptoms, pain patterns, and functional limitations. They may perform specific tests to evaluate nerve function and identify areas of compression.
Physical examination components include:
- Neurological testing to assess reflexes, sensation, and muscle strength
- Range of motion evaluation to identify movement limitations
- Walking assessment to observe gait patterns and symptom reproduction
- Provocative tests that may reproduce symptoms to confirm the diagnosis
Advanced Imaging Studies
Modern imaging technology provides detailed visualization of spinal structures, enabling precise diagnosis and treatment planning.
Magnetic Resonance Imaging (MRI) serves as the gold standard for diagnosing spinal stenosis. MRI provides excellent soft tissue contrast, clearly showing nerve compression, disc problems, and ligament thickening without radiation exposure.
Computed Tomography (CT) scans offer superior bone detail and may be used when MRI is contraindicated or to better visualize bony changes contributing to stenosis.
X-rays help identify structural abnormalities, alignment issues, and degenerative changes but cannot show soft tissue compression directly.
Specialized Diagnostic Tests
In some cases, additional tests may be necessary to fully evaluate the extent of nerve involvement:
- An electromyography test records muscle electrical signals to see if nerves are functioning properly.
- This test measures how effectively your nerves carry electrical messages.
- CT myelography combines CT scanning with contrast dye injection for detailed nerve visualization
Comprehensive Treatment Options: From Conservative to Surgical
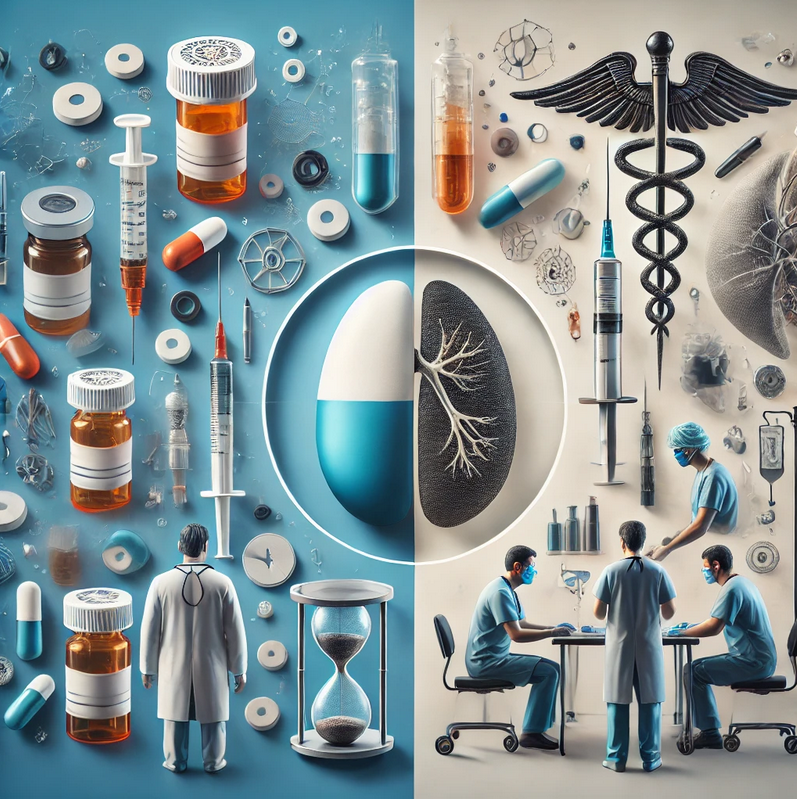
Treatment often begins with less invasive approaches, like medications or physical therapy, and moves to surgery only if necessary. The goal is to relieve symptoms, improve function, and enhance quality of life while minimizing risks.
Conservative Treatment Approaches
Most patients with spinal stenosis initially benefit from non-surgical treatments. These approaches focus on symptom management, functional improvement, and slowing disease progression.
Physical therapy forms the cornerstone of conservative treatment. A skilled physical therapist designs individualized programs focusing on:
- Strengthening exercises for core and back muscles
- Flexibility training to maintain spinal mobility
- Posture education to reduce symptom-provoking positions
- Walking programs with proper pacing and positioning
Medications play a supportive role in symptom management:
- Anti-inflammatory drugs (NSAIDs) reduce inflammation and pain
- Muscle relaxants help alleviate muscle spasms
- Neuropathic pain medications address nerve-related discomfort
- Topical preparations provide localized relief
Injection therapies offer targeted relief for many patients:
- These injections deliver medication right where inflammation is occurring to help reduce pain and swelling.
- Facet joint injections address arthritis-related pain
- Nerve blocks can provide diagnostic information and therapeutic relief
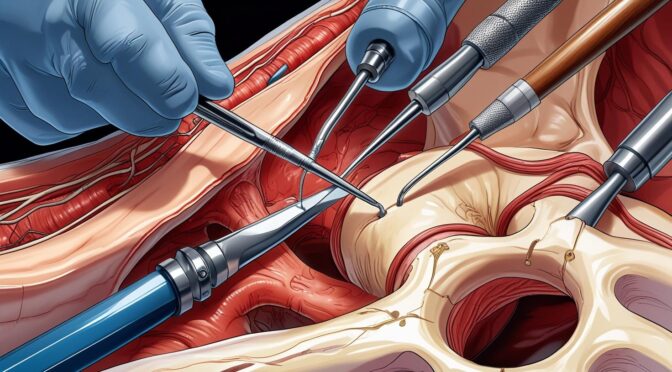
Surgical Treatment Options
Surgery may be considered when other treatments haven’t provided enough relief. Modern surgical techniques offer excellent outcomes with reduced risks compared to traditional approaches.
Decompressive laminectomy represents the most common surgical procedure for spinal stenosis. This procedure removes portions of bone and ligament to create more space for compressed nerves. The surgery can be performed using minimally invasive techniques, reducing recovery time and complications.
Spinal fusion may be recommended when instability accompanies stenosis. This procedure permanently connects two or more vertebrae to prevent movement that could worsen nerve compression.
Minimally invasive procedures continue to evolve, offering patients options with smaller incisions, reduced tissue damage, and faster recovery times. These techniques include endoscopic decompression and percutaneous procedures.
Emerging Treatment Modalities
Research continues to advance treatment options for spinal stenosis. Regenerative medicine approaches, including stem cell therapy and platelet-rich plasma injections, show promise for some patients. Additionally, newer surgical techniques and implant technologies continue to improve outcomes.
Living Successfully with Spinal Stenosis
Managing spinal stenosis extends beyond medical treatment to encompass lifestyle modifications that can significantly impact symptoms and quality of life. Patients who actively participate in their care often achieve better outcomes and maintain independence longer.
Activity modification doesn’t mean stopping all activities but rather adapting them to minimize symptoms. Using assistive devices like walking aids can help maintain mobility while reducing discomfort. Many patients find that activities allowing forward flexion, such as using a shopping cart or stationary bike, become more comfortable than walking upright.
Weight management plays a crucial role in reducing stress on the spine. Even modest weight loss can significantly decrease symptoms and improve mobility. A balanced diet rich in anti-inflammatory foods supports overall spinal health.
Regular follow-up care ensures optimal management and early detection of any changes in condition. Healthcare providers can adjust treatment plans as needed and monitor for potential complications.
Conclusion
Spinal stenosis doesn’t have to define your limitations or dictate your quality of life. By recognizing early warning signs, seeking appropriate medical evaluation, and exploring comprehensive treatment options, you can take control of your spinal health journey.
Recognizing the problem early and managing it promptly makes a big difference. Whether through conservative treatments like physical therapy and medications or advanced surgical interventions when necessary, effective solutions exist for managing spinal interventionism’s and maintaining an active lifestyle.
Remember Sarah, the teacher we mentioned earlier? Through proper diagnosis and a comprehensive treatment plan combining physical therapy, targeted injections, and lifestyle modifications, she returned to walking those school hallways with confidence and comfort.
Don’t let spinal stenosis symptoms go unaddressed. If you’re experiencing persistent back or leg pain, numbness, or walking difficulties, schedule a consultation with a spine specialist today. Early intervention can make all the difference in your treatment outcomes and long-term quality of life.
Book Your Consultation Today – Take the first step toward better spinal health and reclaim your active lifestyle.