Imagine waking up one morning with excruciating pain shooting down your leg, making it nearly impossible to stand or walk. For millions of people suffering from herniated discs, this scenario becomes an unwelcome reality that significantly impacts their quality of life. When conservative treatments like physical therapy, medications, and injections fail to provide relief, spine surgery often becomes the next consideration.
Two primary surgical approaches dominate the landscape of herniated disc treatment: traditional discectomy and microdiscectomy. Both procedures aim to relieve pressure on compressed nerves by removing problematic disc material, yet they differ significantly in technique, recovery time, and overall patient experience. Understanding these differences becomes crucial when facing one of life’s most important healthcare decisions.
The choice between microdiscectomy vs discectomy isn’t always straightforward. Factors such as the size and location of your herniated disc, your overall health status, surgeon expertise, and personal preferences all play vital roles in determining the most appropriate treatment path. This comprehensive guide will walk you through everything you need to know about both procedures, helping you make an informed decision alongside your healthcare team.
We’ll explore the fundamental differences between these spine surgery options, examine their respective benefits and risks, discuss recovery expectations, and provide practical guidance for choosing the right approach for your unique situation. By the end of this article, you’ll have the knowledge necessary to engage in meaningful discussions with your spine specialist about your treatment options.
Understanding Herniated Discs and When Surgery Becomes Necessary
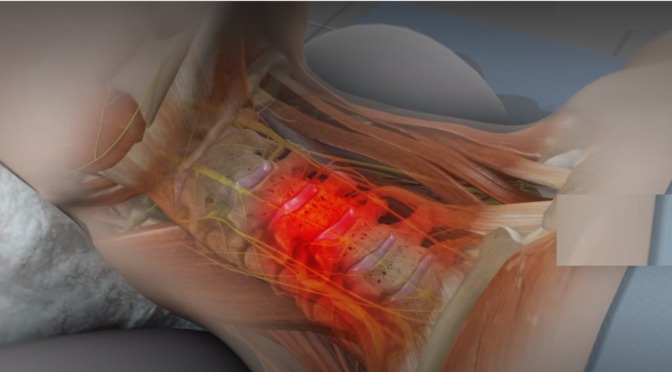
Your spine consists of vertebrae separated by intervertebral discs that act as cushions, absorbing shock and allowing flexible movement. These discs are made up of a jelly-like center called the nucleus pulposus, wrapped by a strong outer layer known as the annulus fibrosus. When the outer layer weakens or tears, the inner material can protrude or “herniate,” potentially pressing against nearby nerves and causing significant pain, numbness, or weakness.
Herniated disc treatment typically begins with conservative approaches. Most patients find relief through a combination of rest, anti-inflammatory medications, physical therapy, and sometimes epidural steroid injections. However, when these non-surgical treatments fail to provide adequate relief after 6-12 weeks, or when patients experience severe neurological symptoms like progressive weakness or loss of bowel/bladder control, surgical intervention becomes necessary.
The decision to pursue spine surgery shouldn’t be taken lightly. Surgeons typically recommend surgical treatment when:
- Conservative treatments haven’t provided relief after a sufficient trial period
- The pain greatly affects daily functioning and overall quality of life
- Neurological symptoms are worsening or severe
- Imaging studies clearly show nerve compression that correlates with symptoms
Both discectomy and microdiscectomy procedures aim to decompress affected nerves by removing the herniated disc material that’s causing pressure. The fundamental goal remains the same: eliminate the source of nerve compression to restore normal function and alleviate pain. However, the surgical approach and techniques used can vary significantly between these two options.
Understanding your specific condition, including the size, location, and severity of your herniated disc, helps determine which surgical approach might be most appropriate. Your spine specialist will consider these factors alongside your overall health, activity level, and treatment goals when recommending the best course of action.
Traditional Discectomy: The Established Approach
Traditional discectomy has served as the gold standard for treating herniated discs for decades. This open surgical procedure involves making a larger incision, typically 2-3 inches long, to provide surgeons with direct visualization and access to the affected disc space. The surgeon removes a portion of the vertebral bone (laminotomy or laminectomy) to reach the herniated disc material and carefully extract the problematic tissue pressing against the nerve.
During a traditional discectomy, patients receive general anesthesia and are positioned face-down on the operating table. The surgeon makes an incision over the affected spinal level, carefully separates the back muscles from the spine, and removes enough bone to access the disc space. Using specialized instruments and direct visualization, the surgeon identifies and removes the herniated disc fragments while taking care to protect surrounding nerves and tissues.
This spine surgery approach offers several advantages, particularly for complex cases. The larger incision provides excellent visualization of the surgical site, allowing surgeons to thoroughly examine the area and remove all problematic disc material. Traditional discectomy works especially well for large herniations, cases involving multiple disc levels, or situations where significant bone removal is necessary to adequately decompress the nerves.
Recovery from traditional discectomy typically involves a hospital stay of 1-2 days, followed by several weeks of activity restrictions. Patients usually experience immediate relief from leg pain, though some temporary back discomfort at the incision site is normal. Physical therapy often begins within a few weeks to help restore strength and mobility.
While traditional discectomy has proven effective over many years, it does involve more tissue disruption compared to minimally invasive alternatives. The larger incision and more extensive muscle dissection can result in increased post-operative pain, longer recovery times, and potentially higher risks of complications such as infection or excessive scar tissue formation.
Microdiscectomy: The Minimally Invasive Revolution
Microdiscectomy represents a significant advancement in spine surgery techniques, utilizing minimally invasive approaches to achieve the same therapeutic goals as traditional discectomy with potentially fewer complications and faster recovery times. This procedure employs a much smaller incision, typically 1-1.5 inches long, combined with specialized instruments and microscopic or endoscopic visualization to remove herniated disc material.
The microdiscectomy procedure begins similarly to traditional surgery, with the patient under general anesthesia and positioned face-down. However, the surgeon makes a much smaller incision and uses a tubular retractor system to create a narrow working channel directly to the affected disc space. This approach minimizes disruption to surrounding muscles and tissues while still providing adequate access to remove the problematic disc material.
Advanced visualization technology plays a crucial role in microdiscectomy success. Surgeons use either an operating microscope or endoscopic camera system to magnify the surgical site, allowing for precise identification and removal of herniated disc fragments. This enhanced visualization often enables more thorough removal of loose disc material while minimizing trauma to healthy tissues.
One of the most significant advantages of microdiscectomy is the reduced tissue trauma compared to traditional approaches. The smaller incision and muscle-sparing techniques typically result in less post-operative pain, reduced blood loss, and faster healing times. Many patients undergoing microdiscectomy can return home the same day or after an overnight hospital stay.
Spine surgery options like microdiscectomy have revolutionized treatment outcomes for many patients. The minimally invasive nature of this procedure often allows for quicker return to normal activities, with many patients resuming desk work within 1-2 weeks and more strenuous activities within 6-8 weeks, depending on their specific situation and healing progress.
However, microdiscectomy may not be suitable for all cases. Very large herniations, complex anatomy, or situations requiring extensive bone removal might still necessitate traditional open approaches to ensure complete treatment and optimal outcomes.
Microdiscectomy vs Traditional Discectomy: A Comprehensive Comparison
When comparing microdiscectomy vs discectomy, several key factors distinguish these spine surgery options and influence treatment decisions. Understanding these differences helps patients and surgeons collaborate in choosing the most appropriate approach for each unique situation.
Surgical trauma and tissue disruption represent perhaps the most significant difference between these procedures. Microdiscectomy involves minimal muscle dissection and tissue disruption, while traditional discectomy requires more extensive exposure and muscle retraction. This difference directly impacts post-operative pain levels, with microdiscectomy patients typically experiencing less discomfort and requiring fewer pain medications.
Recovery time and return to activities vary considerably between these approaches. Microdiscectomy patients often return to light activities within days and resume normal work within 1-2 weeks. Traditional discectomy recovery typically takes longer, with patients needing 2-4 weeks before returning to desk work and 6-12 weeks for more strenuous activities.
Hospital stay requirements also differ significantly. Many microdiscectomy procedures are performed on an outpatient basis or require only overnight observation. Traditional discectomy usually involves a 1-2 day hospital stay, increasing overall treatment costs and potential exposure to hospital-associated complications.
Complication rates tend to favor minimally invasive approaches. Microdiscectomy is associated with lower risks of infection, excessive bleeding, and scar tissue formation. However, both procedures carry similar risks of nerve injury, recurrent herniation, and anesthesia-related complications.
Long-term outcomes for both procedures are generally excellent, with success rates exceeding 85-90% for appropriate candidates. The choice between microdiscectomy vs traditional discectomy often comes down to individual patient factors rather than significant differences in long-term effectiveness.
Cost considerations may favor microdiscectomy due to shorter hospital stays, reduced need for pain medications, and faster return to work. However, the specialized equipment and training required for minimally invasive techniques may offset some of these savings in certain healthcare systems.
Choosing the Right Spine Surgery Option for Your Situation
Selecting between microdiscectomy and traditional discectomy requires careful consideration of multiple factors unique to your specific situation. This decision should always be made in partnership with an experienced spine specialist who can evaluate your individual circumstances and recommend the most appropriate spine surgery approach.
Disc characteristics play a crucial role in surgical planning. Large, complex herniations or those involving multiple levels may require the enhanced visualization and access provided by traditional discectomy. Conversely, smaller, well-contained herniations often respond excellently to microdiscectomy techniques.
Patient anatomy and previous surgical history significantly influence procedure selection. Patients with previous spine surgery, complex spinal anatomy, or significant scar tissue may benefit from the direct visualization offered by traditional approaches. First-time surgical candidates with straightforward anatomy typically make excellent microdiscectomy candidates.
Surgeon expertise and preference cannot be overlooked when choosing between these spine surgery options. While most spine surgeons are trained in both techniques, individual surgeons may have greater experience or comfort levels with specific approaches. Choosing a surgeon with extensive experience in your recommended procedure often matters more than the specific technique used.
Recovery timeline expectations should align with your personal and professional obligations. If you need to return to work quickly or have limited time for recovery, microdiscectomy may offer advantages. However, if thorough treatment is the primary concern regardless of recovery time, traditional discectomy might be preferred for complex cases.
Risk tolerance and personal preferences vary among patients. Some individuals prefer the most minimally invasive option available, while others prioritize the most thorough treatment approach regardless of invasiveness. Discussing these preferences with your surgeon helps ensure your treatment plan aligns with your values and expectations.
Insurance coverage and financial considerations may influence your decision, though most insurance plans cover both procedures when medically necessary. Understanding your specific coverage and any potential out-of-pocket costs helps inform your treatment choice.
The most important factor in choosing between microdiscectomy vs discectomy is finding an experienced spine specialist who can thoroughly evaluate your condition and recommend the most appropriate treatment approach for your unique situation.
Making a Well-Informed Choice About Your Herniated Disc Treatment
The choice between microdiscectomy and traditional discectomy represents an important decision in your herniated disc treatment journey. Both spine surgery options offer excellent outcomes when performed by experienced surgeons on appropriate candidates. Microdiscectomy provides the advantages of minimal tissue disruption, faster recovery, and reduced post-operative discomfort, making it an attractive option for many patients with suitable disc herniations.
However, traditional discectomy remains the preferred approach for complex cases requiring extensive visualization or bone removal. The key to optimal outcomes lies not necessarily in choosing the “best” technique, but rather in selecting the most appropriate approach for your specific condition and circumstances.
We encourage you to engage in thorough discussions with qualified spine specialists, seek second opinions when appropriate, and carefully consider all factors influencing your treatment decision. Remember that successful spine surgery depends on proper patient selection, surgeon expertise, and realistic expectations about recovery and outcomes.
Your journey toward pain relief and restored function begins with taking that first step to consult with a spine specialist who can guide you through these important decisions and help you reclaim your quality of life.