Have you been dealing with persistent neck or back discomfort that worsens when bending, twisting, or standing for long periods? You may be experiencing facet joint syndrome, a common spinal condition that affects the small stabilizing joints between your vertebrae. These joints play a critical role in helping your spine move smoothly, and when they become inflamed or damaged, they can cause significant pain and mobility issues.
Many people assume spinal pain is caused only by disc problems, but facet joint disorders are a leading contributor to chronic spinal discomfort. According to the Cleveland Clinic, facet joint degeneration is one of the most common causes of persistent lower back and neck pain, particularly in aging adults. Without early treatment, symptoms may worsen over time and begin to interfere with daily activities such as sitting, walking, sleeping, or working.
The good news is that pain specialists offer effective, non-surgical approaches to manage this condition and restore spinal function. Early diagnosis, personalized therapy, and targeted interventions can significantly reduce inflammation and improve mobility. In this guide, you will learn the causes, symptoms, diagnostic methods, and advanced treatment options available to help you regain comfort and improve your quality of life.
Understanding Facet Joint Syndrome and Spinal Function
Facet joint syndrome develops when the small joints connecting your vertebrae become inflamed, irritated, or degenerated. These joints are essential for maintaining spinal stability while allowing smooth and controlled movements. When they become damaged, it disrupts normal spinal mechanics and causes localized or radiating pain.
Over time, joint degeneration can worsen due to aging, repetitive stress, or injury. This leads to inflammation, stiffness, and reduced mobility. Understanding how these joints function helps explain why proper care is essential for long-term spinal health and pain prevention.
What Is facet joint syndrome
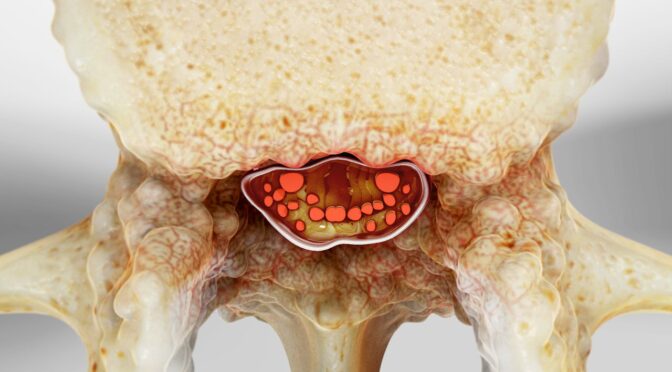
Facet joint syndrome occurs when the cartilage within the spinal facet joints breaks down, leading to inflammation and friction between bones. This condition can affect different regions of the spine, including the neck and lower back, depending on the location of joint degeneration.
As joint damage progresses, movement becomes more difficult and painful. Early detection and treatment help reduce inflammation, improve mobility, and prevent long-term complications.
Key characteristics include:
- Inflammation in spinal joints
- Reduced flexibility
- Pain during movement
- Stiffness after inactivity
How facet joint syndrome Affects Spinal Stability
Facet joints play a crucial role in maintaining proper spinal alignment and movement. When these joints are damaged, the spine becomes less stable, and surrounding muscles must work harder to compensate. This can lead to muscle fatigue, inflammation, and worsening pain over time.
Joint degeneration also increases stress on nearby nerves and tissues. Without treatment, this may result in chronic discomfort and reduced physical function.
Effects on the spine include:
- Increased spinal instability
- Reduced range of motion
- Muscle tension and fatigue
- Higher risk of chronic pain
Recognizing facet joint pain: Symptoms and Warning Signs
Facet joint pain often develops gradually and may initially appear as mild discomfort or stiffness. Many people ignore early symptoms, assuming they are temporary muscle strain. However, untreated joint inflammation can worsen over time and lead to persistent pain.
Recognizing symptoms early allows pain specialists to implement effective treatment strategies. Early intervention reduces inflammation, restores mobility, and prevents long-term complications.
Early Signs of facet joint pain
Early symptoms typically involve localized discomfort in the neck or lower back. Physical movement may intensify the pain, whereas rest can reduce it. These early warning signs are important indicators of joint inflammation.
Ignoring early symptoms may allow the condition to progress and cause more severe discomfort.
Common early symptoms include:
- Localized neck or back discomfort
- Stiffness after sitting or sleeping
- Pain during twisting or bending
- Reduced flexibility
Progressive facet joint pain Symptoms
As inflammation increases, symptoms may become more frequent and intense. Pain can spread to nearby areas such as the shoulders, hips, or upper back. This progression can significantly affect daily activities.
Chronic inflammation may also lead to muscle tension and fatigue, worsening discomfort and mobility limitations.
Progressive symptoms include:
- Radiating pain
- Increased stiffness
- Muscle tightness
- Reduced mobility
When facet joint pain Requires Medical Attention
Persistent symptoms indicate worsening joint damage and require professional evaluation. Early medical intervention helps prevent further degeneration and improves recovery outcomes.
Delaying treatment may result in chronic pain and long-term mobility issues.
Warning signs include:
- Pain lasting several weeks
- Difficulty performing daily activities
- Sleep disturbances
- Increasing pain intensity
Causes and Risk Factors of facet joint syndrome
Facet joint syndrome develops due to multiple factors, including aging, lifestyle habits, and physical stress. These factors accelerate joint degeneration and increase inflammation. Understanding risk factors helps patients take preventive measures.
Addressing these causes early helps reduce symptoms and protect spinal health.
Aging and facet joint syndrome Development
Natural aging causes cartilage to wear down over time. Reduced cartilage increases friction between joints, causing inflammation and pain.
Age-related degeneration is one of the most common causes of spinal joint problems.
Age-related risk factors include:
- Cartilage breakdown
- Reduced joint lubrication
- Increased inflammation
- Joint stiffness
Lifestyle Factors That Increase Risk
Poor posture and inactivity increase stress on spinal joints. Sedentary lifestyles weaken muscles that support the spine, increasing joint strain.
Lifestyle improvements can significantly reduce the risk of joint degeneration.
Lifestyle risks include:
- Poor posture
- Lack of exercise
- Obesity
- Prolonged sitting
Injury and Mechanical Stress
Physical injuries and repetitive movements can damage facet joints. Occupational strain and sports injuries increase the risk of degeneration.
Preventive care reduces injury risk and protects spinal function.
Common injury-related causes include:
- Sports injuries
- Falls
- Heavy lifting
- Repetitive strain
Facet joint treatment: Conservative Treatment Options
Facet joint treatment focuses on reducing inflammation, relieving pain, and restoring spinal mobility. Pain specialists typically begin with non-surgical treatments that are safe and effective. These approaches improve joint function and reduce symptoms.
Early conservative care provides excellent outcomes for most patients.
Physical Therapy as facet joint treatment
Physical therapy strengthens muscles that support the spine. Strong muscles reduce stress on joints and improve spinal stability.
Therapy programs are customized based on individual needs and symptoms.
Benefits include:
- Improved flexibility
- Reduced inflammation
- Better posture
- Increased mobility
Medication-Based facet joint treatment
Medications help control inflammation and reduce discomfort. Pain specialists prescribe medications based on symptom severity.
Medication improves comfort and supports rehabilitation.
Common medications include:
- Anti-inflammatory drugs
- Muscle relaxants
- Pain relievers
- Topical treatments
Lifestyle-Based facet joint treatment
Lifestyle changes support long-term recovery and prevent further damage. Healthy habits reduce joint stress and improve spinal health.
Consistent lifestyle changes enhance treatment outcomes.
Helpful lifestyle changes include:
- Regular exercise
- Weight management
- Proper posture
- Ergonomic adjustments
Advanced facet joint treatment From Pain Specialists
Advanced facet joint treatment options provide relief when conservative care is insufficient. Pain specialists use minimally invasive procedures to reduce inflammation and block pain signals. These treatments offer long-term relief and improved mobility.
Modern interventional treatments are safe, effective, and widely used.
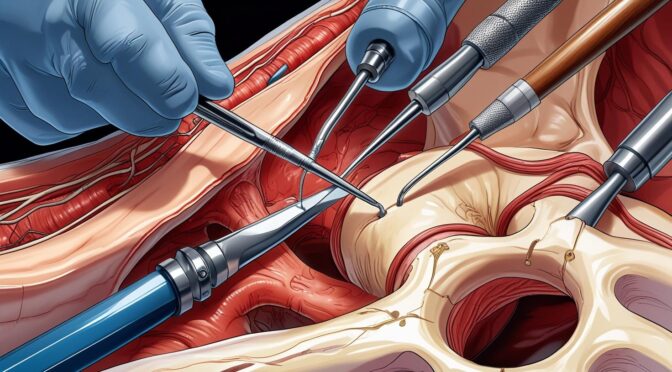
Injection-Based facet joint treatment
Injections deliver anti-inflammatory medication directly into affected joints. This reduces inflammation and relieves pain quickly.
These procedures are minimally invasive and performed by specialists.
Common injection treatments include:
- Corticosteroid injections
- Facet joint injections
- Medial branch blocks
- Diagnostic injections
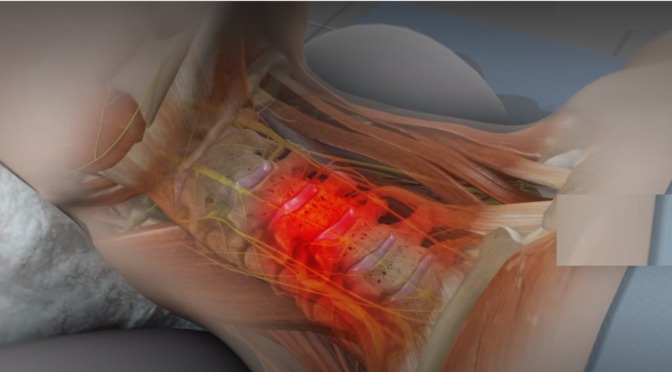
Radiofrequency Ablation facet joint treatment
Radiofrequency ablation blocks pain signals by targeting affected nerves. This treatment ensures long-lasting comfort and greater mobility.
It is recommended for patients with chronic pain.
Benefits include:
- Long-term pain relief
- Improved mobility
- Reduced inflammation
- Minimally invasive treatment
Diagnosis and Specialist Evaluation of facet joint syndrome
Accurate diagnosis is essential for effective treatment. Pain specialists use clinical evaluations and imaging tests to identify joint inflammation and degeneration. Proper diagnosis ensures targeted treatment and faster recovery.
Early evaluation improves treatment success.
Clinical Evaluation of facet joint syndrome
Pain specialists assess symptoms, medical history, and spinal function. Physical examination helps identify joint inflammation and mobility limitations.
Accurate assessment guides treatment planning.
Evaluation methods include:
- Physical examination
- Range of motion testing
- Pain assessment
- Medical history review
Imaging Tests for facet joint syndrome
Imaging tests confirm diagnosis and identify joint damage. These tests help specialists develop personalized treatment plans.
Imaging improves diagnostic accuracy.
Common imaging tests include:
- MRI scans
- X-rays
- CT scans
- Diagnostic injections
Conclusion
Chronic spinal discomfort can significantly affect daily life, but early diagnosis and proper care provide effective relief. Understanding symptoms, causes, and treatment options empowers patients to take control of their spinal health. Pain specialists offer personalized care plans that improve mobility and reduce inflammation. Most importantly, facet joint syndrome can be effectively managed using non-surgical treatments and minimally invasive procedures. Addressing the issue early helps ensure better recovery and sustained relief. Schedule your consultation today to receive expert diagnosis and personalized treatment for lasting spinal pain relief.