What is Laminectomy?
Laminectomy is a surgical procedure that involves the removal of a portion of the vertebra known as the lamina. The lamina is part of the vertebral arch, a bony structure that protects the back side of the spinal cord. By removing this section, surgeons can relieve pressure on the spinal cord and nerves, which can be caused by a variety of factors such as herniated discs, spinal stenosis, or bone spurs. This procedure is often recommended when conservative treatments like medication or physical therapy fail to alleviate symptoms.
The primary goal of a laminectomy is to create more space within the spinal canal, allowing for the decompression of nerves and the spinal cord. This decompression can significantly reduce symptoms such as pain, numbness, and weakness that often accompany nerve compression in the spine. Laminectomy can be performed on different parts of the spine, including the cervical, thoracic, and lumbar regions, depending on where the pressure is occurring.
While the concept of removing a part of the vertebral bone might sound daunting, laminectomy is a well-established procedure with a long history in spinal surgery. Advances in surgical techniques and technology have made it a safe and effective option for many patients. Understanding the specifics of how laminectomy works can alleviate fears and misconceptions about the procedure, paving the way for more informed decision-making regarding spinal health.
Indications for Laminectomy
Laminectomy is typically indicated for individuals experiencing significant nerve compression in the spine, which can manifest as chronic back pain, sciatica, or neurological symptoms. One of the most common conditions leading to a laminectomy is spinal stenosis, a narrowing of the spinal canal that increases pressure on the nerves. This condition often results from age-related changes in the spine, such as the thickening of ligaments, bone spurs, or bulging discs.
Another indication for laminectomy is the presence of herniated discs, where the inner gel of a disc protrudes through its outer layer, pressing on nearby nerves. While many cases of herniated discs can be managed with non-surgical interventions, surgery becomes necessary when symptoms persist or worsen, significantly impacting the patient’s quality of life. Other indications include tumors, cysts, or injuries that compromise the spinal canal’s integrity.
Deciding on a laminectomy involves a thorough evaluation by a healthcare professional, including a detailed medical history, physical examination, and imaging studies such as MRI or CT scans. These assessments help determine the precise cause and location of the nerve compression, ensuring that surgery is the most appropriate and effective treatment option. Patients should engage in open discussions with their medical team to fully understand the reasons for recommending laminectomy and to explore any alternative treatments available.
Benefits of Laminectomy
One of the primary benefits of undergoing a laminectomy is the relief from chronic pain that has been resistant to other forms of treatment. By alleviating pressure on the spinal cord and nerves, patients often experience significant reductions in pain, allowing them to return to daily activities they may have previously avoided. This pain relief can lead to improved mobility and overall well-being, as patients can engage in physical activities without the fear of exacerbating their symptoms.
Laminectomy can also contribute to the restoration of neurological function. Nerve compression can lead to symptoms such as tingling, numbness, and muscle weakness, which can severely impact a person’s ability to perform routine tasks. By decompressing the affected nerves, laminectomy can help restore normal sensation and muscle strength, improving a patient’s ability to function independently and enhancing their quality of life.
Beyond physical benefits, laminectomy can have positive psychological effects. Chronic pain and disability can lead to feelings of frustration, depression, and anxiety. Successful surgery often results in a renewed sense of hope and motivation, as patients regain control over their bodies and lives. While the decision to undergo surgery is never taken lightly, the potential benefits of a laminectomy can be life-changing for those who have exhausted other treatment avenues.
Potential Risks and Complications
As with any surgical procedure, laminectomy carries potential risks and complications that patients should be aware of before making a decision. One of the primary concerns is the risk of infection, which can occur at the surgical site or within deeper tissues. Surgeons take extensive precautions to minimize this risk, including the use of sterile techniques and, in some cases, prescribing antibiotics before and after the procedure.
Bleeding and blood clots are other potential complications associated with laminectomy. While significant bleeding during the procedure is uncommon, it can occur, leading to the need for a blood transfusion or additional interventions. Blood clots, particularly in the legs, can also develop post-surgery, posing a risk of pulmonary embolism if they travel to the lungs. Patients are often encouraged to move around soon after surgery to promote circulation and reduce the likelihood of clot formation.
Nerve damage is a rare but serious complication of laminectomy. Although the procedure is intended to relieve pressure on the nerves, there is a small risk of accidental damage during surgery, which can result in new or worsening symptoms. Additionally, some patients may experience issues related to anesthesia, such as allergic reactions or respiratory problems. Understanding these risks and discussing them with the surgical team can help patients make informed decisions and prepare for potential outcomes.
The Laminectomy Procedure Explained
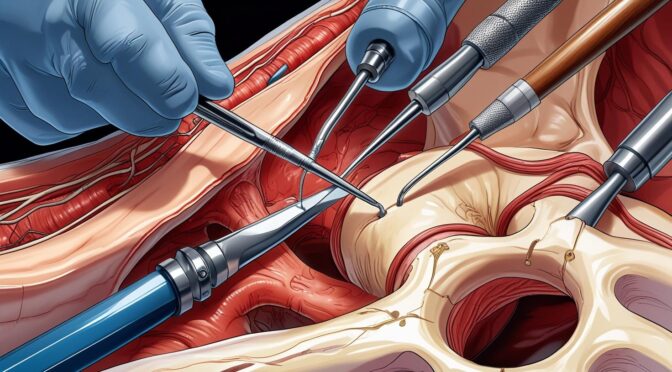
The laminectomy procedure is typically performed under general anesthesia, ensuring that the patient is unconscious and free of pain during the surgery. The patient is positioned face-down on the operating table, allowing the surgeon access to the affected area of the spine. Once the patient is properly positioned, the surgical team prepares the site by cleaning it with antiseptic solutions to prevent infection.
The surgeon makes an incision over the affected vertebrae, carefully moving aside muscles and tissues to expose the spine. Using specialized instruments, the surgeon removes the lamina, creating more space within the spinal canal. Depending on the specific condition being treated, additional procedures may be performed, such as removing herniated disc material or excising bone spurs. In some cases, a spinal fusion may be recommended to stabilize the spine if significant bone is removed.
Once the decompression is complete, the surgeon closes the incision with sutures or staples and covers it with a sterile dressing. The entire procedure can take several hours, depending on the complexity and extent of the surgery. After the operation, patients are moved to a recovery room, where they are monitored as they awaken from anesthesia. Understanding each step of the laminectomy procedure can help alleviate concerns and prepare patients for what to expect on the day of surgery.
Recovery Process After Laminectomy
Recovery from a laminectomy can vary widely among patients, depending on factors such as age, overall health, and the complexity of the surgery. Initially, patients may experience some discomfort and swelling at the surgical site, which is a normal part of the healing process. Pain management is a crucial aspect of recovery, with medications prescribed to help control discomfort in the days following the surgery.
Patients are typically encouraged to begin moving soon after the procedure to promote healing and reduce the risk of complications such as blood clots. Gentle walking and physical therapy exercises can help improve circulation and prevent stiffness. While it may be tempting to rest extensively, early mobilization is essential for a smooth recovery and can expedite the return to normal activities.
The timeline for returning to work and other activities varies, with some patients able to resume light duties within a few weeks, while others may require a more extended period of recovery. Regular follow-up appointments with the surgeon are important to monitor progress and address any concerns that may arise. By adhering to post-operative instructions and actively participating in the recovery process, patients can optimize their outcomes and achieve the best possible results from their laminectomy.
Pain Management and Rehabilitation
Effective pain management is a cornerstone of successful recovery after laminectomy. In the immediate post-operative period, patients are likely to be prescribed a combination of medications to manage pain and inflammation. These may include opioids for severe pain, nonsteroidal anti-inflammatory drugs (NSAIDs), and muscle relaxants. It’s essential for patients to follow their prescribed medication regimen and communicate with their healthcare provider about any side effects or concerns.
Rehabilitation plays a critical role in restoring function and strength after laminectomy. Physical therapy often begins shortly after surgery and is tailored to the individual needs of the patient. A physical therapist will guide patients through exercises designed to improve flexibility, strength, and stability in the spine. As recovery progresses, the intensity and complexity of exercises are gradually increased to match the patient’s capabilities.
In addition to professional rehabilitation, patients are encouraged to incorporate gentle activities into their routines, such as walking, swimming, or yoga, as tolerated. These activities can enhance cardiovascular health, improve mood, and accelerate the healing process. By actively engaging in both formal rehabilitation and personal activities, patients can facilitate a smoother recovery and reduce the risk of future spinal issues.
Lifestyle Changes Post-Surgery
Adopting healthy lifestyle changes after laminectomy can significantly impact long-term outcomes and prevent recurrence of symptoms. One of the most important changes is maintaining a healthy weight, as excess body weight can place additional stress on the spine and hinder recovery. Patients should focus on a balanced diet rich in nutrients, including protein, vitamins, and minerals, to support tissue healing and overall health.
Incorporating regular exercise into daily life is another crucial lifestyle change. While the type and intensity of exercise should be tailored to individual abilities and recovery progress, staying active can help maintain spinal flexibility and strength, reducing the likelihood of future issues. Patients should consult with their healthcare providers or physical therapists to develop a safe and effective exercise plan that meets their needs.
Smoking cessation is particularly important for individuals recovering from laminectomy, as smoking can impair blood flow and delay healing. Quitting smoking not only benefits spinal health but also improves overall cardiovascular and respiratory health. By embracing these lifestyle changes, patients can enhance their recovery, support spinal health, and improve their quality of life long after surgery.
Frequently Asked Questions About Laminectomy
Patients considering laminectomy often have numerous questions about the procedure, recovery, and long-term outcomes. One common question is how long the effects of the surgery will last. While laminectomy can provide significant relief from symptoms, its longevity varies depending on the underlying condition and adherence to post-surgery recommendations. Some patients experience long-lasting relief, while others may require additional treatments in the future.
Another frequently asked question is whether laminectomy will limit physical activities. Post-surgery, patients are encouraged to gradually resume activities, with modifications as necessary. While some high-impact sports or activities may need to be adjusted, most patients can return to a full range of activities with appropriate precautions and conditioning. Consulting with healthcare providers about specific activities can ensure a safe and effective return to an active lifestyle.
Patients may also wonder about the potential for surgery to be unsuccessful. While laminectomy is generally effective in relieving symptoms, there is a possibility that some patients may not experience the desired outcome. Factors such as the extent of nerve damage or the presence of other spinal issues can influence results. Open communication with the surgical team and realistic expectations are essential components of the decision-making process.
Conclusion and Next Steps
Understanding laminectomy, from its indications and benefits to potential risks and recovery insights, is crucial for anyone considering this surgical option. By comprehensively exploring this procedure, patients can make informed decisions about their spinal health and confidently navigate their treatment journey. Laminectomy offers a promising path to relief for many individuals suffering from chronic back pain and neurological symptoms, enabling them to reclaim their quality of life.
For those considering laminectomy, the next steps involve a thorough discussion with healthcare providers, including surgeons and rehabilitation specialists, to evaluate the appropriateness of the procedure based on individual circumstances. Patients should feel empowered to ask questions, seek second opinions, and explore all available treatment options to ensure the best possible outcome.
Ultimately, laminectomy can be a transformative experience, providing significant relief and improved function for those struggling with debilitating spinal conditions. By approaching the decision with knowledge and preparation, patients can embark on the path to recovery with confidence, supported by a comprehensive understanding of what to expect before, during, and after surgery.