Understanding Foraminotomy: A Comprehensive Guide to Relief from Nerve Compression
What is Foraminotomy?
Foraminotomy is a surgical procedure designed to relieve nerve compression in the spine, specifically targeting the foramen. The foramen is a small opening between the bones in the spine through which nerve roots exit. When these openings become narrowed, either due to bone spurs, herniated discs, or other spinal conditions, it can compress the nerves, leading to pain, numbness, and weakness. Foraminotomy involves enlarging this passageway to alleviate the pressure on the affected nerves.
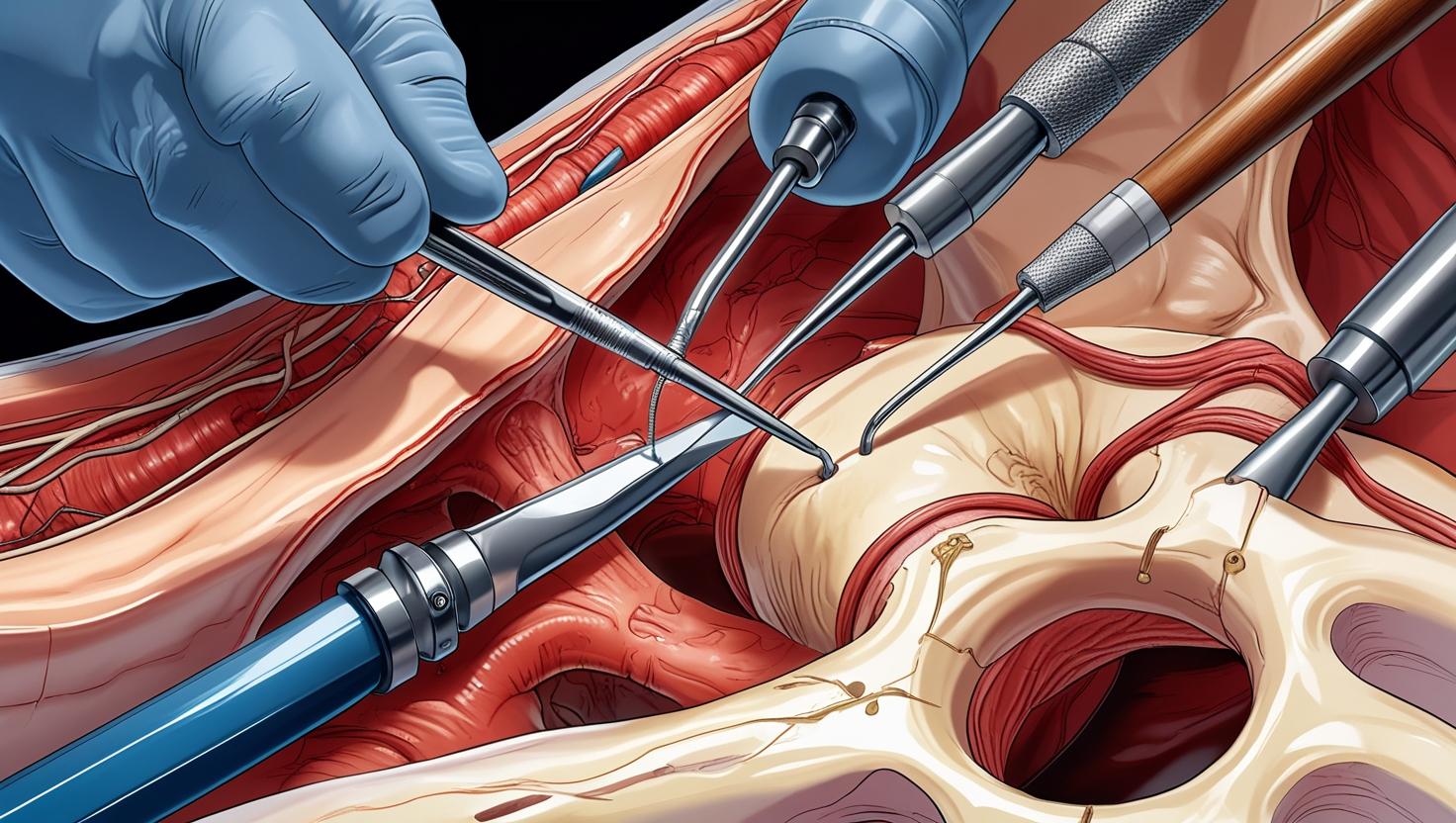
This minimally invasive surgery is often performed using advanced techniques that require only small incisions, reducing recovery time and minimizing risks compared to traditional open surgery. Surgeons typically use specialized instruments and imaging technology to guide the procedure with precision. The primary goal is to remove the source of compression while preserving as much of the natural anatomy as possible. This approach not only leads to pain relief but also helps maintain spinal stability.
Foraminotomy can be an effective solution for individuals who have not found relief through conservative treatments such as physical therapy, medication, or spinal injections. It offers a targeted approach to resolving nerve compression issues while minimizing collateral damage to surrounding tissues. Understanding the specifics of this procedure is crucial for patients considering it as a potential pathway to alleviate debilitating symptoms.
The Anatomy of Nerve Compression
Nerve compression occurs when excessive pressure is placed on a nerve by surrounding tissues, such as bones, cartilage, muscles, or tendons. In the context of spinal health, this pressure often arises from changes in the structure of the spine, including the narrowing of the foraminal canals. This narrowing, medically known as foraminal stenosis, can result from various degenerative conditions, impacting the normal functioning of spinal nerves.
The spinal column is a complex structure made up of vertebrae, intervertebral discs, ligaments, and nerve roots. The nerve roots exit the spinal column through the foramina, serving as conduits for nerve signals traveling between the spinal cord and the rest of the body. When these foramina are constricted, the nerve roots can become compressed, leading to a range of symptoms, from localized pain to radiating discomfort that follows the path of the nerve.
Understanding the anatomy involved in nerve compression is essential for recognizing the potential benefits of foraminotomy. By addressing the specific areas where compression occurs, foraminotomy aims to restore the normal function of the affected nerves. This targeted approach not only alleviates symptoms but also prevents further deterioration of the spinal structure, promoting long-term spinal health.
Common Causes of Nerve Compression
Several factors can contribute to the development of foraminal stenosis and subsequent nerve compression. One of the most common causes is degenerative disc disease, a condition wherein the intervertebral discs lose their cushioning ability over time. As the discs degenerate, they can bulge or herniate into the foraminal space, exerting pressure on the nerve roots and causing pain.
Another prevalent cause of foraminal narrowing is the formation of bone spurs, or osteophytes. These bony projections often develop as a natural response to degeneration or arthritis, as the body attempts to stabilize the spine. However, the growth of these spurs can encroach upon the foramina, leading to compression of the nerves. Other conditions, such as arthritis or scoliosis, can also contribute to foraminal stenosis by altering the structural integrity of the spine.
Traumatic injuries, such as fractures or dislocations, can further exacerbate nerve compression by altering the alignment of the spinal column. Additionally, lifestyle factors, including poor posture, obesity, and lack of physical activity, can increase the stress on the spine, potentially leading to or aggravating foraminal stenosis. Understanding these causes is vital for prevention and for determining when surgical intervention like foraminotomy may be necessary.
Symptoms Indicating the Need for Foraminotomy
Recognizing the symptoms of nerve compression is critical for determining the appropriate course of treatment. Common indicators that may suggest the need for foraminotomy include persistent pain in the back or neck that radiates into the arms or legs. This pain is often accompanied by numbness, tingling, or weakness in the extremities, which can significantly impact daily activities and overall quality of life.
Patients may also experience a loss of motor function or coordination, making it difficult to perform tasks that require fine motor skills. In severe cases, nerve compression can lead to muscle atrophy or changes in reflexes, further highlighting the need for medical evaluation. The intensity and location of these symptoms can vary depending on the specific nerves affected and the degree of compression.
It is essential for individuals experiencing these symptoms to seek medical consultation. A thorough evaluation, which may include imaging studies such as MRI or CT scans, can help identify the exact cause and location of nerve compression. This diagnostic process is crucial for determining whether foraminotomy is a viable option and ensuring the best possible outcome for the patient.
The Foraminotomy Procedure: What to Expect
Undergoing a foraminotomy involves several stages, beginning with a preoperative assessment to evaluate the patient’s overall health and suitability for surgery. This assessment typically includes a review of medical history, physical examination, and imaging studies to confirm the diagnosis of nerve compression. Once deemed a suitable candidate, the patient is scheduled for the procedure, which is usually performed on an outpatient basis.
During the operation, the surgeon makes a small incision near the affected area of the spine. Using specialized instruments and real-time imaging guidance, the surgeon carefully removes the bone or tissue causing the compression. The goal is to enlarge the foramina and relieve pressure on the nerve roots without compromising the stability of the spine. This precision minimizes trauma to the surrounding tissues and promotes faster healing.
Post-operatively, patients are monitored for a brief period before being discharged. Recovery instructions are provided, including guidelines for pain management, activity restrictions, and follow-up appointments. While the surgery itself is relatively quick, typically lasting one to two hours, the preparation and recovery processes are equally important in achieving successful outcomes.
Benefits of Foraminotomy for Nerve Compression Relief
Foraminotomy offers several significant benefits for individuals suffering from nerve compression. One of the primary advantages is the relief of pain and other debilitating symptoms, allowing patients to resume their normal activities with reduced discomfort. By directly addressing the source of compression, foraminotomy provides targeted relief that can significantly improve the patient’s quality of life.
The minimally invasive nature of the procedure means that patients often experience shorter recovery times and less postoperative pain compared to traditional open surgeries. The use of small incisions reduces the risk of infection, scarring, and other complications, making foraminotomy a safer option for many patients. Additionally, the preservation of spinal stability is a critical benefit, as it helps maintain the overall function and alignment of the spine.
Beyond physical improvements, foraminotomy can also have positive psychological effects. The reduction of chronic pain and restoration of mobility can lead to improved mental health and well-being. Patients often report increased energy levels and a more active lifestyle following successful foraminotomy, highlighting the comprehensive benefits of this surgical intervention.
Risks and Complications Associated with Foraminotomy
As with any surgical procedure, foraminotomy carries certain risks and potential complications. While the surgery is generally considered safe, it is important for patients to be aware of these risks to make informed decisions. Common complications include infection, bleeding, and adverse reactions to anesthesia, though these are relatively rare due to the minimally invasive nature of the procedure.
Nerve damage is another potential risk, albeit infrequent. Given the proximity of the surgical site to the spinal nerves, there is a small chance of injury during the procedure, which could lead to worsening of symptoms or new neurological deficits. Surgeons take great care to minimize this risk by using advanced imaging techniques and specialized instruments to guide their movements with precision.
Other complications may include cerebrospinal fluid leaks or recurrence of symptoms if the underlying cause is not fully addressed. It is crucial for patients to discuss these risks with their healthcare provider, weighing them against the potential benefits of the surgery. A thorough understanding of the procedure and its associated risks allows patients to approach foraminotomy with confidence and realistic expectations.
Recovery and Rehabilitation After Foraminotomy
The recovery process following foraminotomy is a critical component of achieving successful outcomes. Patients are typically encouraged to engage in a rehabilitation program that includes physical therapy and exercises designed to strengthen the spine and improve flexibility. These activities are tailored to the individual’s needs and progress, gradually increasing in intensity as the patient heals.
Pain management is an integral part of the recovery phase, with medications prescribed to alleviate discomfort and inflammation. Patients are advised to adhere to activity restrictions to prevent strain on the surgical site. This may include avoiding heavy lifting, twisting movements, and prolonged periods of sitting or standing during the initial weeks of recovery.
Regular follow-up appointments with the healthcare provider are essential to monitor the healing process and address any concerns that may arise. These visits provide an opportunity to assess the effectiveness of the surgery, adjust rehabilitation plans, and ensure that the patient is on track for a full recovery. With proper care and adherence to postoperative instructions, most patients can expect to return to their normal activities within a few months.
Alternative Treatments for Nerve Compression
While foraminotomy is an effective solution for many individuals with nerve compression, it is not the only treatment option available. Conservative approaches, such as physical therapy, chiropractic care, and pain management techniques, are often recommended as initial interventions. These methods aim to alleviate symptoms and improve function without the need for surgery.
For some patients, spinal injections, including epidural steroid injections, can provide temporary relief by reducing inflammation and swelling around the affected nerve. These injections are typically used in conjunction with other treatments to enhance their effectiveness and provide longer-lasting benefits. Additionally, lifestyle modifications, such as weight management, ergonomic adjustments, and exercise programs, can play a significant role in managing symptoms and preventing further deterioration.
In cases where conservative treatments fail to provide adequate relief, other surgical options may be considered. Procedures such as laminectomy, discectomy, or spinal fusion may be appropriate depending on the specific cause and location of the nerve compression. It is important for patients to explore all available options and work closely with their healthcare providers to determine the most suitable approach for their condition.
Conclusion: Is Foraminotomy Right for You?
Deciding whether foraminotomy is the right choice involves careful consideration of various factors, including the severity of symptoms, the underlying cause of nerve compression, and the patient’s overall health. For individuals who have not achieved relief through conservative treatments, foraminotomy offers a promising solution with its minimally invasive approach and targeted effectiveness.
Potential candidates should engage in open discussions with their healthcare providers, weighing the benefits and risks associated with the procedure. Understanding the specifics of the surgery, including the recovery process and long-term outcomes, is crucial for making informed decisions. Additionally, exploring alternative treatments and considering second opinions can provide a comprehensive view of available options.
Ultimately, the decision to undergo foraminotomy should be based on a thorough evaluation of individual needs and goals. With the right approach and support, foraminotomy can pave the way towards a pain-free future, restoring mobility and enhancing quality of life for those affected by nerve compression.